While breastfeeding is natural, it can be difficult for some at first. It may take time and practice. Be patient and give yourself and your baby time to get comfortable with breastfeeding. Try following these three steps to help you get started, and check out our other pages on solving common problems.
If sitting, you can use a pillow to take the weight of your baby at first so your arms are rested. If lying back, use cushions or pillows to support your back and shoulders. If lying on your side, place a pillow under your head. Below are some pictures of a range of positions you can try.

Two things will help your baby get a good latch; 1. Baby’s mouth should cover as much of the areola (dark part of breast) as possible. 2. Her bottom lip and tongue must get to your breast first, and should touch your areola as far from the base of the nipple (the part that protrudes from the center of your areola) as possible. To latch baby onto your breast: 1) Bring baby to your breast, (not breast to baby) with her head facing your nipple, her nose (not mouth) in line your nipple. This way your baby will naturally tip her head back just before she latches on. 2) Make sure she has a wide open mouth and is leading with her chin. 3) Once her mouth is on your areola, her lips should be flanged and chin tucked. The following pictures show how to get a good latch.

Instruction source: Babycenter.co.uk
Image source:https://bundleofcare.files.wordpress.com/2014/07/latchon4images.jpg
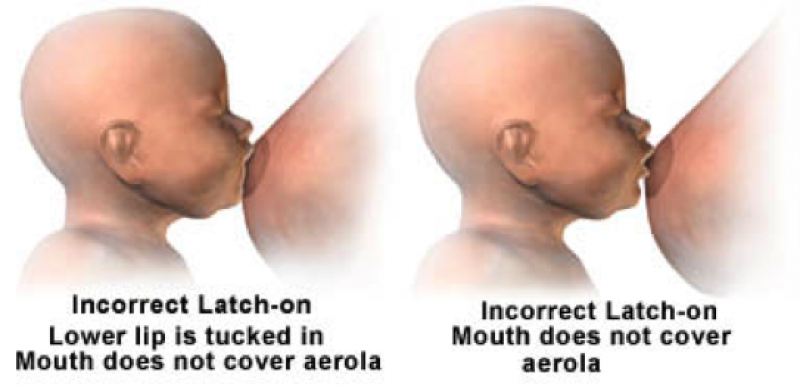
The two pictures below show examples of a bad latch.

You can also watch the videos below to show how to get a good latch.
While it’s always best to let baby finish each breast when they want to, if you need to stop, don’t just pull baby off as this might hurt your nipple. Just insert a finger in the corner of your baby’s mouth or gums to break the suction.

While breastfeeding is natural, it can be difficult for some at first. It may take time and practice. Be patient and give yourself and your baby time to get comfortable with breastfeeding. Try following these three steps to help you get started, and check out our other pages on solving common problems.
If sitting, you can use a pillow to take the weight of your baby at first so your arms are rested. If lying back, use cushions or pillows to support your back and shoulders. If lying on your side, place a pillow under your head. Below are some pictures of a range of positions you can try.

Two things will help your baby get a good latch; 1. Baby’s mouth should cover as much of the areola (dark part of breast) as possible. 2. Her bottom lip and tongue must get to your breast first, and should touch your areola as far from the base of the nipple (the part that protrudes from the center of your areola) as possible. To latch baby onto your breast: 1) Bring baby to your breast, (not breast to baby) with her head facing your nipple, her nose (not mouth) in line your nipple. This way your baby will naturally tip her head back just before she latches on. 2) Make sure she has a wide open mouth and is leading with her chin. 3) Once her mouth is on your areola, her lips should be flanged and chin tucked. The following pictures show how to get a good latch.
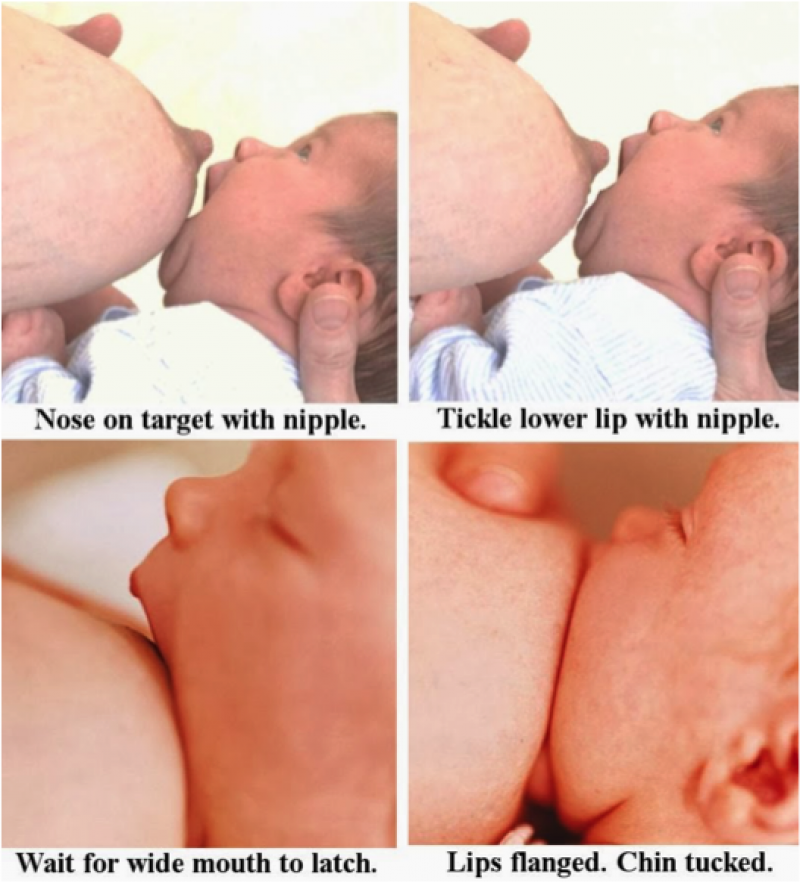
Instruction source: Babycenter.co.uk
Image source:https://bundleofcare.files.wordpress.com/2014/07/latchon4images.jpg
The two pictures below show examples of a bad latch.
You can also watch the videos below to show how to get a good latch.
While it’s always best to let baby finish each breast when they want to, if you need to stop, don’t just pull baby off as this might hurt your nipple. Just insert a finger in the corner of your baby’s mouth or gums to break the suction.

Picture source: March of Dimes,
http://www.marchofdimes.org/materials/how-to-breastfeed.pdf
It is a good idea to burp your baby when you change breasts, especially if they spit up often or have uncomfortable gas. Burp your baby midway through the nursing if she seems uncomfortable during nursing (squirming, pulling away or crying). Below are three different burping positions you can try.

Over the shoulder
On lap
Sitting up
Instructions source: www.babycenter.com
Really Good Drinking: shows a baby who is drinking very well. Look for the pause in the chin as baby opens his mouth to the maximum, just before closing his mouth, indicating his mouth is filling up with milk. The longer the pause, the more milk the baby is taking in.
Nibbling: shows a baby that is doing almost no drinking. A baby who breastfeeds only with this type of sucking could stay on the breast for hours and still not get enough milk.
28 Hour Old Assisted Latching: shows latching on that isn’t perfect, but good enough. It takes two tries to get the baby to latch on, but that’s okay; there’s no point in trying to force a baby to stay on the breast. It won’t work. Compressions help the baby get more milk.
28 Hour Old Baby-Led Mother Guided Latching: shows how you can adjust and improve the latch even if it doesn’t start great. The mother does not bring baby on very well and so the baby has a shallow latch. The mother starts compressing and baby responds by having pausing-type sucks that indicate he is getting milk well.
|
Age |
Nursing Characteristics
|
|
0 to 2 weeks |
Nursing habits: you should nurse on demand i.e. whenever and for however long your baby likes. Typically should feed every 3-4 hours (8-12 times per day) for 20 minutes each breast (although baby can go an hour or more). If baby is drowsy and falls asleep on the breast within a few minutes, wake her up so she can continue eating. Once baby is finished with first breast, offer second breast but don’t worry if she will not take it. “Cluster feeding”, where nursings cluster together often at certain times during the day, is common. Diaper output: in the first week, one wet diaper per each day of life and one stool per each day of life up to day 3-5. In second week, 4-6 wet diapers, 3-6 stools per day. Stools during first few days are black and tarry, but lighten to a yellowy mustard color by day 5. Stool consistency is often like peanut butter or cottage cheese, and smell is usually quite mild. To ensure baby is getting enough milk, it is more important to track number and type of stools than number of wet diapers. Weight gain: baby should return to birth weight within two weeks (newborns lose 7-10% of birth weight in first 48 hours). |
|
2 to 6 weeks |
Nursing habits: continue to nurse on-demand and as often as you want to. Baby can go longer between feeds but should nurse around 8 times every 24 hours. But don’t ‘watch the clock’ and nurse when your baby wants to. Some babies nurse much more often than others either because the baby is more efficient at getting milk or the mother produces more milk. Nursing frequently will help your milk supply. Cluster feeding is still common at this age. Babies start to become more efficient and nursing time often shortens. Diaper output: 5-6 wet diapers, 3-4 stools per day. Urine should be pale in color and not smelly. Stools should be mustardy color and soft-to-runny in consistency. Weight gain: Typically babies gain 170gms per week, but your baby may gain more or less. Your baby’s doctor will monitor weight gain. |
|
6 weeks to 4 months |
Nursing habits: you are likely to have ‘hit your stride’ with breastfeeding and your baby is also becoming more efficient and feeding at more regular times. Feed baby 6-8 times every 24 hours. Diaper output: at about 6 weeks, baby’s stool output drops dramatically to around 1 per day, however babies can often go several days or even a week without a bowl movement. This happens because breastmilk leaves very little solid waste to be eliminated from baby’s digestive system. It is not a reason to add formula, teas, prune juice or other foods to the baby’s diet. Try extra nursings, and also massaging his belly gently and bicycling his legs. Weight gain: average weight gain continues to be 170gms per week but your baby’s doctor will monitor weight gain. Birth weight is usually doubled by 4-6 months. Use the WHO’s growth chart provided here to track your baby’s progress. |
|
4 to 9 months |
Nursing habits: you have become even more proficient at breastfeeding and it will often take only five minutes. How often you nurse depends on your baby, but the number is likely to decline over this time. Babies will likely be more fidgety and touchy, and this can be bothersome, so distract them before it becomes a habit. Diaper output: same as previous. Weight gain: between 4-7 months this will slow to around 120gms per week, and from 7-9 months to around 80gms per week. Use the WHO’s growth chart provided here to track your baby’s progress. |
|
9 to 18 months |
Nursing habits: some feedings might be as short as a few minutes and the amount of times will vary greatly by child, but mostly it will start to decline. Most babies are eating solid foods by now although some may not start until up to 12 months. As solids become an increasingly important aspect of baby’s diet, your breastmilk supply will likely decline, but baby will still get most of his essential nutrition from your breastmilk. Weight gain: will slow between 9-12 months to about 65g per week. Use the WHO’s growth chart provided here to track your baby’s progress. |
|
Toddlers |
Nursing habits: frequency and length will vary greatly by child; some will want frequent nursings while others only one or twice a day. Your milk supply will likely keep pace with your child’s needs. If your toddler is sick or stressed she will likely nurse more often. Weight gain: use the WHO’s growth chart provided here to track your child’s progress. |
Breast compressions help by pushing more milk into baby’s mouth and turning baby’s sucking/nibbling into drinking. The technique may be useful for:
Watch how to breast compressions here.
You will not always need to do this. As breastfeeding improves, you will be able to let things happen naturally.